Preventing Infection Outbreaks During Disaster Recovery
From HVAC to sanitation systems, facility managers need to keep occupants healthy while housed in emergency shelters
By Jake Meister, Contributing Writer
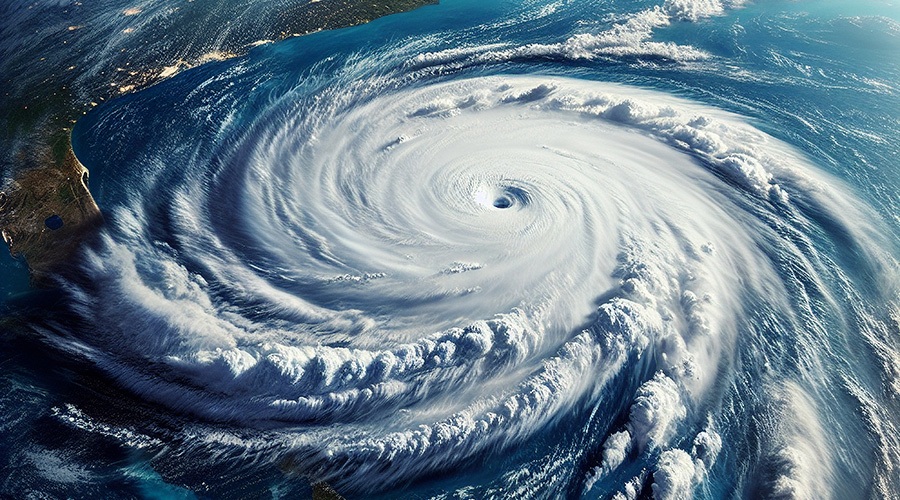
The United States experienced 28 natural and climate disasters costing at least $1 billion in 2023, surpassing the record of 22 set in 2020, according to the National Oceanic and Atmospheric Administration. These disasters present a significant opportunity for an infectious outbreak as many people gather in shelters before, during, and after a storm. Considering the increased likelihood of a major disaster in many parts of the country, facility managers responsible for potential shelters must have a plan in place.
Some of the first actions facility managers should do is identify potential problem areas within their facility. That’s because facilities used during natural disaster emergencies are often hurriedly fashioned into a makeshift shelter. If problems aren’t identified beforehand, it’s likely a problem would be too difficult to address once the time comes. One area of initial emphasis should be HVAC and ventilation.
“People that are in facilities don’t have the big infrastructure with HEPA machines and such like a hospital,” says Barabara Smith, infection preventionist at Mount Sinai St. Luke’s and Mount Sinai West hospitals in New York an author for the Association for Professionals in Infection Control and Epidemiology’s (APIC) recently updated “Infection Prevention and Control for Shelters During Natural Disasters.”
Smith says facility managers need to know what their ventilation can and can’t do. They must be aware how much of the ventilation can be manipulated to meet needs. They should also know where the air is coming from and where it is discharged to.
Another point of emphasis is sewage and sanitation systems because any use of a facility for emergency sheltering purposes will deviate from the norm. People staying at an emergency shelter will often use the sinks to wash clothing, so people supervising the facilities must keep an eye out for that problematic behavior. Also, toilets will get considerable use, so restrooms must be consistently cleaned and monitored, minimizing the spread of sickness in those areas. Finally, there should be a plan in place to ensure adequate water supply for not only the cleaning, but for potential human consumption.
Smith suggests putting a plan in place for where people will be escorted into the facility during an emergency as that will be one of the first courses of action during the event. The entrances should be controlled and people placed into two locations. One location will be used to place people who are contagious, and another should be used for those demonstrating no symptoms. There should also be a designated place for both regular waste and medical waste to be placed, since typical disposal methods will unlikely be an option. There should also be a designated place for linens, all of which should be handled with gloves.
If possible, facilities will obviously want to have energy during the emergency, so facility managers should check to see that any generator at the facility is up to date with fueling.
Other tips include:
- Having instructions in pictorial form in the event of issues with language gaps.
- Handle all linen with gloves.
- If possible, monitor co-mingling of people at the shelter. Discourage the practice of sharing blankets.
- Follow local department of health recommendations regarding the use of masks.
- Reach out to other community operators (the local health department, fire department, emergency management group, and community partners) now to know what resources they will have in the event of an emergency.
Jake Meister is a freelance writer in Milwaukee, Wisconsin.
Related Topics: