How to Prepare for a Natural Disaster During a Pandemic
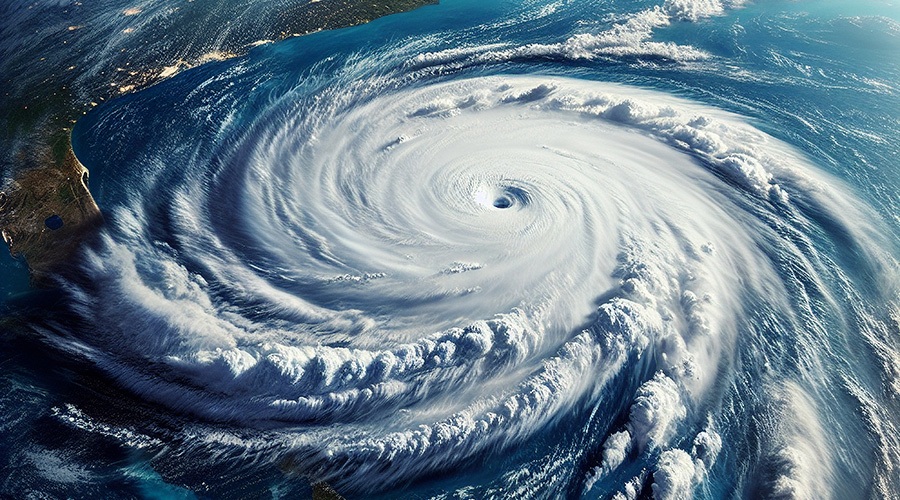
As wildfires rage and an extremely active hurricane season continues - all during a pandemic - it's imperative to have a well-polished and effective emergency management plan.
Healthcare workers and hospitals continue to fight on the frontlines of the COVID-19 pandemic. While the number of cases has begun to trend downward, new crises are moving to the forefront of facility directors’ minds: wildfires and hurricanes. As clinicians focus on patients, it is the facilities teams that must be prepared for multiple disasters that could strike. How can hospitals juggle all these crises at once?
Over the coming weeks, CDC forecasts estimate “1,600 to 7,000 new COVID-19 hospitalizations per day.” At the same time, the United States is in the middle of its annual hurricane season, which has been deemed “extremely active” for 2020. In California, wildfires have burned more than 1.8 million acres at the time of this writing, with record-breaking heatwaves further intensifying outbreaks.
It’s not luck that will keep our hospitals and other healthcare facilities in impacted areas functional, but preparation. Hospitals are a critical infrastructure asset for the community and need to provide care to those in need before, during or after a disaster, if it’s weather-related or not.
Facilities must routinely research and update plans in order to reduce damage, remain open and recover quickly to withstand the shattering effects of hurricanes, wildfires and the global pandemic.
Emergency Management Program
It is imperative to have a well-established emergency management (EM) program to lay the foundation to successfully address any unexpected crises, especially in the U.S. where many healthcare facilities fall short in disaster planning and preparedness. Planning for, responding to and recovering from a crisis is a multi-disciplinary effort, and the strength of an EM program and its team lies in the ability to help a facility through coordinating responses, planning through the disaster, and maintaining safety in times of uncertainty.
For hurricanes and wildfires or other events that move through an area, a detailed Emergency Management plan should cover monitoring threats and risks; equipment staging; assessments for wind, water or smoke damage; operations during the event, and post-event recovery. For the pandemic, consider including information on negative pressure rooms, controlling HVAC and other systems remotely, CDC guidance, supply chain management, signage and space reconfiguration, and more. Incorporating these details and prioritizing them based on the emergency or emergencies occurring will be crucial to reducing damage and costs while successfully maintaining operations.
In addition to event-related Emergency Management plans, success comes with experience developed through general EM planning and implementation, and relationships built at local, state, national and global levels. To create a successful program, it’s important to not just create one with the goal of meeting minimum regulatory requirements or saving money, but rather ensuring all facilities are prepared to serve their communities during great times of need, no matter what emergency.
Leadership
Clear, strong leadership for EM programs is paramount. Managing this program should not fall as a mere bullet point in a facility team’s job description but should be designated a high-importance responsibility. More ideal, a facility’s preparedness is even better served by having an EM team designate an additional group of subject matter experts to tackle problems both within the facility and the multi-system organization as a whole. With this team, members can prepare guidance and navigate communication channels as they act as a liaison between the EM team, patients and staff. It’s important to gather top experts in a variety of fields – engineering, EM, operations, technology, construction, facilities management – to ensure all bases are covered.
Working in a variety of fields means the experts will be able to monitor facilities’ activity and adapt quickly to any situation in real-time during an emergency. This diverse team can collaborate and create solutions for facilities to adjust processes and programs to ensure safety. Maintaining this team even after the current emergency is crucial. Set up quarterly meetings with this group of experts to collaborate on and update existing plans, review new resources and inspire fresh ideas for the EM team.
For weather-related events, leadership will play an integral role in decision making. Critical decisions, such as procuring additional resources and planning patient evacuation, need to be made at least 48 hours before landfall for a hurricane and 72 hours when in proximity to wildfires, even as a full impact area and intensity are unknown. The leadership team will also be responsible in determining staffing plans, canceling elective procedures, and closing off-site locations. Decisions should be coordinated with other hospitals in the impact area, as well. For example, if one hospital chooses to evacuate patients 48 hours ahead of a hurricane’s landfall, while another does not, that will greatly impact a community and its residents.
Communication
Communication is essential for proper disaster preparedness. Whether communicating with staff, patients, government agencies, or the public, healthcare facilities should establish these channels early. Staff communication in particular should be determined as part of the planning process to understand which staff may be available to assist during a disaster and any needs they may have, such as child or family care.
Patient and family communication is also critical, especially during COVID-19 when patients may be unable to receive in-person visitors. In the event of natural disasters, if patients’ families need to evacuate the area, the hospital’s ability to continue to communicate with them about the patient is vital. Patients, as well, should understand there is a plan to continue to provide care and keep them safe. If patients are evacuated, communicating with family members on where they are being moved and how to contact them is key.
Communicate early, often and accurately through regular updates, especially when there are a multitude of sources for the public to receive information. Control the conversation by utilizing a single expert source to provide regular communication on facility response, updates on the outbreak or storm, and guidance to your facility teams.
Evaluate and Update
Regardless of how an Emergency Management plan was or was not implemented during a year, plans should be revisited and updated annually. After an emergency, a thorough after-action review should be completed, including input from staff, patients and community response organizations. If any corrective actions are needed, a specific corrective plan should be written with leaders and timelines assigned. Once the corrective plan is completed, the updated plan should be tested through exercise, and staff should be reeducated on any changes to the plan.
We are currently living through an above-average hurricane season, an over-active wildfire season, and a global pandemic. Healthcare facilities are in a unique position to safeguard patients, staff and communities through all of these emergencies. Ensure your facility is prepared to weather the storm, no matter what it is.
Scott Cormier is the vice president of emergency management, environment of care (EOC) and safety at Medxcel. Cormier leads the development and implementation of emergency management, general safety and accident-prevention programs for a national network of hospitals.
Related Topics: