How Hospitals Use Energy
First of a two-part article on the intersection of energy efficiency and patient satisfaction in healthcare facilities.
When thinking about how to reduce energy use in hospitals, one of the first questions to ask is: Where do hospitals use energy today? The follow-up question is: What are the greatest targets for energy efficiency and how can they be addressed in a way that maintains functionality and patient comfort in the healthcare environment?
One of the best resources for understanding how energy is used in hospitals comes from a study conducted by the University of Washington Integrated Design Lab in conjunction with Solarc A+E at the Legacy Salmon Creek Hospital in Vancouver, Wash., published in 2012. What follows is a breakdown of the particular uses.
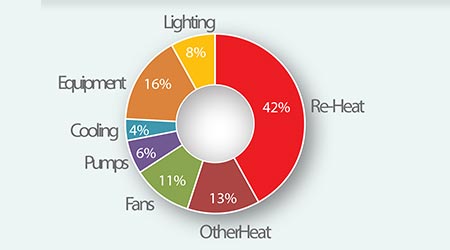
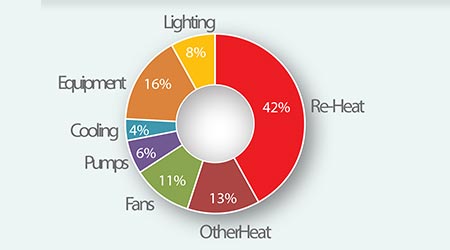
(Caption: The chart shows a breakdown of energy consumption at the Legacy Salmon Creek Hospital in Vancouver, Wash. Source: Washington Integrated Design Lab, http://128.95.168.21/t100/CAS_LSC.php)
Reheat. Much of the reheat energy use is driven by the conventional practice of over-chilling incoming air to drive moisture out of it, then re-heating it as needed for thermal comfort in VAV boxes. VAV is a system that is intended to deliver both comfort and ventilation as part of the same system. The need to heat up the air at the room level partly stems from the practice of minimizing the number of supply air temperature zones in a facility. In addition, VAV boxes don’t have the ability to cool air, and can only heat the air that comes to them. In other words, if an entire floor of a bed tower is being supplied with one air temperature, through a single duct, the fact that VAV can only heat means that the supply air temperature needs to be lowered to cool the hottest spaces on the floor (typically those over-exposed to solar heat load), while every other space must have the air heated back up to serve their tempering comfort needs.
Over-chilling and additional reheat can be thought of as energy wastes.
Other heat. Steam heating and wastes associated with line losses and inefficiencies in a central steam system to kitchen and process uses (sterilization, autoclaves) are notable in this category. When it’s possible to replace old central steam systems with distributed steam generation, it’s worth studying whether or not current technology can meet the needs of the facility. In an era where the negative community health impacts of combustion and production of greenhouse gasses are entering the public consciousness, the opportunity to eliminate boilers and move to increasingly clean electricity is also worth studying. An all-electric building in Seattle, for instance, has virtually no carbon footprint.
Boilers also generate the hot water typically used in reheat, although at a temperature higher than is absolutely needed.
Fans. Fan energy is largely driven by air handlers and the need to deliver sufficient air to meet code air change rates. It’s common that greater than the required air change capacity is built into building systems, because the peak load, usually driven by solar cooling demands is what sets the size, and therefore the cost of the mechanical cooling system. Note that recent changes to ASHRAE standards have reduced the required air changes for medical/surgical rooms.
Pumps and cooling. Much of the pump energy is connected to the movement of fluids, including those used in the cooling system of the hospital. Much of the cooling is tied to the initial dehumidification of incoming air. Note that this category may actually account for more energy consumption in a higher performance hospital.
Equipment. Imaging equipment accounts for only 0.9 percent of the total energy graph — so the vast majority is miscellaneous equipment, such as distributed refrigeration in kitchens, ice machines, and dietary rooms.
Lighting. Lighting is a dynamic consumption area. LED lighting was not commonly used in hospitals when the Legacy Salmon Creek Study was conducted, and lighting controls were not incorporated into the base facility.
Patient experience
Comfort in patient rooms is often managed using very old technology. Of the many factors that influence comfort, only ambient air temperature is measured by thermostats. This means that the comfort implications of air velocity and radiant hot or cold surfaces are not accounted for in this metric. In reality, an exposed window surface can make the family zone too cold or too hot, and the velocity of air delivered through the ceiling register may create an uncomfortable draft. In the end, the functional way that comfort is measured is through feedback via calls to the nurse when patients can’t get comfortable.
When patients are consistently uncomfortable, the hospital facility team will do what it takes, despite the system constraints, to make patients comfortable. This priority suggests that energy conservation goals are likely to be sacrificed if the system design doesn’t accommodate adjustment for comfort.
Additional components of comfort include glare avoidance, while providing quality daylight, shown to be a component in returning to health. If it’s too bright and blinds get closed, daylight becomes unavailable to the patient, so the design must be carefully modeled to avoid glare. Of course daylight provides another benefit, which is that interior lighting can be dimmed when there is enough outside light. Balancing the light in the room through dimming can also reduce the electrical consumption of lighting.
Off-gassing from surface treatments, cleaning products and odors in the air due to recirculation can also make a hospital feel antiseptic and separated from a natural or homelike environment. Air quality as an issue should be strongly considered against safety concerns when considering the patient experience, such as in the case of employing operable windows.
Related Topics: